Acute Pain Vs Chronic Pain
Pain is something which is experienced by all and can be very uncomfortable. The International Association for the Study of pain define pain as " An unpleasant sensory and emotional experience association with actual or potential tissue damage, or described in terms of such damage".
Pain is also based on an individual experience and can be categorized as acute and chronic pain.
Acute pain usually has a duration of 12 weeks. It usually has a sudden onset from a known cause. It is an adaptive mechanism of the body to promote healing and recovery. Chronic pain occurs after 12 weeks. It is a long lasting pain and may arise from a particular injury that did not heal or an underlying cause. However there may not be an underlying cause.
Pain can also present as Hyperalgesia (exaggerated response to noxious stimulus), or Alloydina ( pain generated from a normal stimulates that doesn't usually cause pain such as clothes rubbing on skin).
|
Acute Pain |
Chronic Pain |
|
Less than 12 weeks |
More than 12 weeks |
|
Causes usually known |
Cause usually unknown |
|
Usually self limiting |
Long lasting duration |
|
Automatic response: Hyperactivity |
Automatic response: Often absent |
|
Anxious, restfulness |
Flat mood, depressed |
|
Visible changes such as swelling, bruisng etc |
Visible changes such as deformity, muscles wasting etc |
Pain Pathway
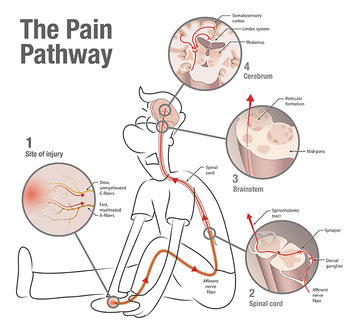
Firstly we need to understand the pain pathway:
Site of Injury
A noxious event has been recognized as pain by a conscious person. The pain signals are carried thorough different afferent nerve fibers to the central nervous system. The slow unmyelinated C fibers transmit a broad range of stimulus such as mechanical, thermal, or metabolic.
The fast myelinated A-fibers respond to mechanical or thermal stimulus by producing a sharp sense of pain.
Spinal Cord
Once afferent nerve fibers are stimulated, an action potential is created to transmit pain signals to the dorsal horn of the spinal cord. Here a further synapse occurs and transmits to the thalamus and brain stem.
Cerebrum
Nociceptive impulses are relayed to multiple areas of the brain including somatosensory cortex, the insula and the limibic system
Classification of pain
Identifying the type of pain will assist with the treatment protocol. The most common types of pain are:
Nociceptive Pain
Is a normal response of the nerves being stimulated by injury or damage such as sprain, burns, inflammation etc. The nerves transmit pain to the brain via the peripheral nervous system. The pain is usually localized and is like a constant dull ache. It is usually time limited as pain ceases when the damaged tissue heals. Typically seen in acute pain.
Neuropathic Pain
Is result of injury or malfunction of the peripheral or central nervous system. It can be triggered by injury, but may not be due to damage to the nervous system. The pain usually presents as a burning or electric shock type of feeling. It can also cause sensory abnormalities. This type of pain is commonly seen in chronic pain, as pain signals are constantly firing. Examples of this are diabetic neuropathy, entrapment neuropathy (i.e carpal tunnel syndrome), peripheral nervous system (widespread nerve damage).
Inflammatory Pain
Mediators within the body are released at the area of tissue inflammation causing the activation of the nocicpetive pain pathway. Therefore taking precautions to reduce the inflammation will effect the pain sensation level. Examples of this are appendicitis, Rheumatoid Arthritis, inflammatory bowel disease etc.
However in many cases there can be a complex mixture of nocicpetive and neuropathic factors such as migraine pain, myofascial pain etc.
Assessment
An assessment of a patient in pain is multidimensional in order to provide an effective treatment strategy. In order to do this the Chiropractors will carry out the following:
- Taking a full history, including physical and neurological screening.
- If the clinician feels necessary, referral for further imaging such as xrays, MRI, blood tests etc.
- Psychosocial assessment to assess any psychological factors contributing to pain management.
- Patient explanation of findings, diagnosis, treatment options and prognosis.
- Advice on activity, lifestyle, rehabilitation, self-management etc.
- Monitoring and re-assessing when required.
Self-management tips

Being in pain can be disabling and prevent daily activities.
Therefore the following information may assist with self management of pain until you consult your GP or Chiropractor:
Acute Pain
- PRICE (protection, rest, ice, compress and elevate).
- Find your pain free movements and try to avoid any painful movements.
- NSAIDS, over counter pain killers (always read label).
- Use support aids.
Chronic Pain
- Heat is generally more effective for Chronic pain.
- Relaxation techniques using deep breathing.
- Exercise.
- Behavioral changes.
- Muscle relaxants
The above listed are not conclusive to the type of pain, and you may find that you do not fit into a particular area. Therefore it is important to seek professional health if you are experiencing pain.
Seeing a Chiropractor for Pain
Chiropractors specialise in assessing, diagnosing and managing conditions of the spine. They are highly trained in finding the cause of pain in the spine. In the UK they undergo a minimum of four years’ full-time training. Importantly, chiropractors are regulated by law and must work within strict professional and ethical boundaries.
Before starting treatment, a chiropractor will do a full assessment. This will involve taking details about your condition, current health and medical history, and performing a physical examination. Sometimes it may be necessary to refer you for other tests, such as X-rays, MRI scans or blood tests. It is important for your chiropractor to gather as much information about your back pain as possible so that the most precise diagnosis can be made.
Your chiropractor will then explain what is wrong, what can be done and what you can expect from chiropractic treatment.
Chiropractors are best known for manual treatments such as spinal manipulation, where they use their hands to free stiff or restricted joints, or mobilisation, which is the gradual moving of joints.
But they may also use other recommended treatments such as certain types of acupuncture, electrotherapy, stretching exercises and rehabilitation, all of which form part of a chiropractor’s package of care. Your chiropractor may also offer lifestyle advice to help recovery and to prevent repeated episodes of back pain.
If your chiropractor does not think you can be helped by chiropractic treatment, you may be referred back to your GP or to another health professional. Chiropractors do not prescribe medication, so if this is needed, you may be referred back to your GP. As chiropractors support a joined-up approach to care, they may ask if they can send a brief report to your GP.
Many people who suffer long-term back pain benefit from regular, supportive chiropractic care to reduce the risk of recurrent episodes.
Other treatments that might help with pain management available at TWC:
As with any new symptoms it is always important to visit your GP or Chiropractor to rule out any other disorders before reaching a diagnosis yourself.
